We Must Learn To Treat Dual Diagnosis
Professions in the field can best provide treatment for addiction. They can do this because they utilize various behavioral therapies and clinical expertise. This is especially true of individuals who need to treat dual diagnosis. According to the National Survey on Drug Use and Health , 45 percent of people with addiction have a co-occurring mental health disorder. By examining the definition of dual diagnosis, common dualities, and current methods of treatment, one can feel confident in seeking professional assistance, as it is necessary in treating this condition.
What is Dual Diagnosis?
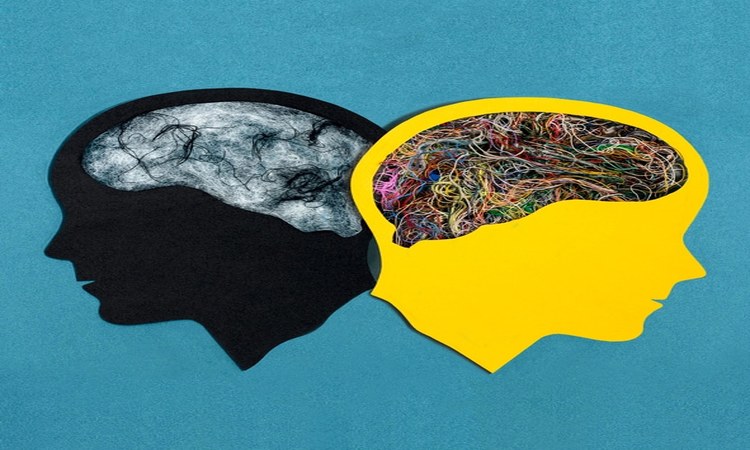
Dual diagnosis is a term professionals use to describe the event in which an individual has a substance use disorder and a mental health disorder diagnosis simultaneously. The origin of a dual diagnosis varies. Some individuals suffering from a mental health disorder turn to substances as a way to self-medicate, while others have developmental disorders as a result of their substance abuse. Due to the psychological nature of a dual diagnosis, this condition is extremely common within the addiction and recovery community, with almost half of the members reporting a diagnosis of coexisting disorders.
Common Dual Diagnoses
While we exclude no disorder, neither mental or physical, from the dual diagnosis model, there are several dualities that are most common within the addiction and recovery community. Due to the effects of substance addiction on brain chemistry, the most common dual diagnoses tend to revolve around mental health. The most common diagnoses that come with substance abuse and addiction are depression, anxiety, Post-Traumatic Stress Disorder (PTSD), and Bipolar Disorder.
Depression and Addiction
As one of the most common mental illnesses throughout the world, depression is often a coexisting disorder in those struggling with addiction. As many addictive substances act as depressants, using them long-term can often lead to chronic depression as a result of irreversible chemical imbalances in the brain. Likewise, those struggling with depression often feel the urge to self-medicate and do so by abusing addictive substances which eventually leads to addiction.
Anxiety and Addiction
While there are various forms of anxiety, those who suffer from this disorder share a common feeling of restlessness or unease. Oftentimes, anxiety sufferers begin relying on sedative-type substances in order to relieve these symptoms. Common drugs of abuse among those with anxiety include alcohol, opioids and benzos due to their relaxing effects.
PTSD and Addiction
Post Traumatic Stress Disorder, commonly known as PTSD, is a form of severe anxiety brought on by a traumatic event or a series of traumatic events. Common PTSD sufferers include, but are not limited to, military veterans, survivors of abuse, and survivors of natural disasters. As with anxiety sufferers, those with PTSD often develop substance addictions as a means to numb feelings of grief or block memories of trauma. Some individuals with PTSD may also have a physical injury. Therefore, they may rely on addictive substances to relieve pain.
Bipolar Disorder and Addiction
Bipolar Disorder characterizes itself by extreme and sudden changes in mood or temperament. Addiction is common among those suffering from Bipolar Disorder. The reason for this is because people often rely upon substances to control or stabilize their mood, thereby providing temporary relief. However, once this temporary relief fades away, substance abuse can provoke symptoms of Bipolar Disorder.
Signs That Someone Has Coexisting Disorders
Similar to any substance addiction, there are indicators that suggest an individual may be struggling with coexisting disorders and has yet to receive a dual diagnosis from a medical professional. If an individual uses an addictive substance in excess and displays any of the following signs, they likely suffer from addiction and a concurrent mental disorder. These signs include:
- Poor performance at school or work
- Loss of appetite
- Isolation
- Insomnia
- Excessive fatigue or lethargy
- Depression
- Anxiety or fear
- Suicidal Ideation
- Extreme, uncontrollable mood swings
- Lapses in memory
- Financial stress
- Family history of coexisting disorders
How To Treat Dual Diagnosis
When treating a dual diagnosis, a specialist is essentially treating two separate disorders. There is a correlation between mental illness and addiction. However, each disorder must have individual treatment. The individual treatment generates the most favorable outcome for the person who has the diagnosis. Treatment for addiction and mental illness are very similar, yet there are a few key differences.
Treating A Mental Illness
Mental disorders in those who have a dual diagnosis are typically either the result of drug abuse or the source of drug abuse. Regardless of the means, mental health is an extremely important component in terms of overall health and wellbeing. Within a dual diagnosis treatment plan, professionals address mental disorders through various therapies and medication, if necessary. The same professionals often use individual and holistic therapies to confront past trauma. They work with the patient to develop healthy behaviors and thought processes. Medication can effectively alleviate symptoms of the mental disorder, as well. In concurrence with receiving addiction treatment, patients receive support in setting new goals towards a rewarding and sober life.
Treating An Addiction
Similar to treating mental illness, addiction treatment for an individual with coexisting disorders is vital for overall recovery and health. Clinicians highly recommend that those suffering from addiction or a dual diagnosis enter a professional addiction treatment program. These establishments provide specialists with expertise and training in their fields. These specialists can help a great deal along the road to recovery. Professional addiction treatment strategies incorporate various behavioral therapies. Some of these therapies include cognitive-behavioral therapy, individual and group therapy, and motivational therapy, among others. These talk therapies work to identify the root source of addiction. They also confront past trauma, and establish new, healthy behavioral thought patterns. Depending on the individual’s addiction, medication-assisted treatment may also be available to assist in preventing cravings.
You Are Not Alone
Dual diagnosis is the event of having two coexisting disorders. It is very common among the addiction and recovery community. Nearly half of its populace report mental health disorders alongside addiction. While this condition can become serious and life-threatening if someone doesn’t get treatment, there are scientifically proven ways to treat dual diagnosis. By seeking professional help, you can receive treatment for mental illness and addiction simultaneously via therapies and medication.
Now you know the definition of dual diagnosis, common dualities, and current methods of dual diagnosis treatment. You can prepare yourself to tackle this disorder knowing that you are not alone. Our experts are here and awaiting your call. If you or a loved one is suffering from a dual diagnosis, call us today and take the first step on your road to recovery.
